- Your cart is empty
- Continue Shopping

Why ExoBrite™ Outperforms PKH and Carbocyanine Dyes
Discover reliable EV labeling beyond PKH. Explore Biotium’s ExoBrite™ stains for accurate, reproducible extracellular vesicle analysis.

Exosome therapy holds immense promise, particularly in areas such as regenerative medicine, oncology, and drug delivery. However, it remains in its infancy. Academic researchers aiming to bring their discoveries to the clinic must overcome critical translational hurdles, chief among them: quality control (QC) for regulatory readiness.
Today, exosome-based products are often offered through private clinics, typically marketed without regulatory approval. The U.S. FDA has issued warnings that no exosome therapy is currently approved, citing concerns over inconsistent manufacturing and a lack of quality standards.
Academic innovators must recognize that demonstrating therapeutic potential alone is insufficient. Commercializing exosomes-based products demands robust systems for consistency, safety, and compliance, and QC is the cornerstone of this transition.
Exosomes, a subtype of extracellular vesicles (EVs), are heterogeneous biological nanoparticles, secreted by cells and carrying molecular cargo such as proteins, lipids, and RNAs.
These features make them therapeutically powerful—but also difficult to standardize.
These challenges have necessitated the use of advanced stabilization technologies, yet comprehensive evaluation is still needed to confirm that exosomes retain their original characteristics after processing and storage.
Sterility testing is a fundamental QC requirement and a cornerstone of ensuring the safety of any biologic or cell-derived therapeutic product, including exosome-based therapies. Regulatory agencies such as the US FDA, European Medicines Agency (EMA), and other global authorities mandate stringent sterility and biosafety testing before approving products for clinical use. This requirement spans the entire development lifecycle from early-phase investigational products to commercialized therapies.
Exosomes are typically harvested from conditioned media of cultured producer cells. Because the production environment involves prolonged in vitro culture, complex purification steps, and manipulation of biological fluids, there is an inherent risk of contamination by bacteria, fungi, mycoplasma, or adventitious viruses. These contaminants can be introduced during raw material sourcing, handling, processing, or packaging and may not be entirely removed by downstream purification processes such as ultracentrifugation, tangential flow filtration (TFF), or size-exclusion chromatography.
Therefore, sterility testing is not merely a regulatory checkbox; it is a critical safety gate to ensure that the final exosome drug product does not pose infectious risks to patients. Contaminants in injectable EV preparations could result in severe adverse reactions, including sepsis, fever, or immune responses, especially given their frequent intravenous route of administration.
These are standard for cell-based therapies and biologics and are expected to apply equally to EV-based therapeutics:
| Test | Method | Purpose |
| Mycoplasma | Culture method | Detects contaminating mycoplasma species |
| Bioburden | Membrane filtration | Measures viable microbial content |
| Adventitious viruses | In vitro assays (cytopathic effect, hemagglutination, hemadsorption) | Screens for unknown viral contaminants |
| Sterility | Direct inoculation | Confirms absence of live microorganisms |
| Endotoxin | Gel clot or photometric LAL test | Detects bacterial endotoxins, critical for IV administration |
Academic researchers moving into translational development of exosome-based therapeutics often face a steep learning curve when it comes to regulatory-grade safety testing, especially around sterility and microbial safety. Unlike preclinical research where basic aseptic techniques may suffice, therapeutic development demands validated, regulatory-compliant sterility and biosafety protocols.
Below are key areas academic researchers should pay special attention to:
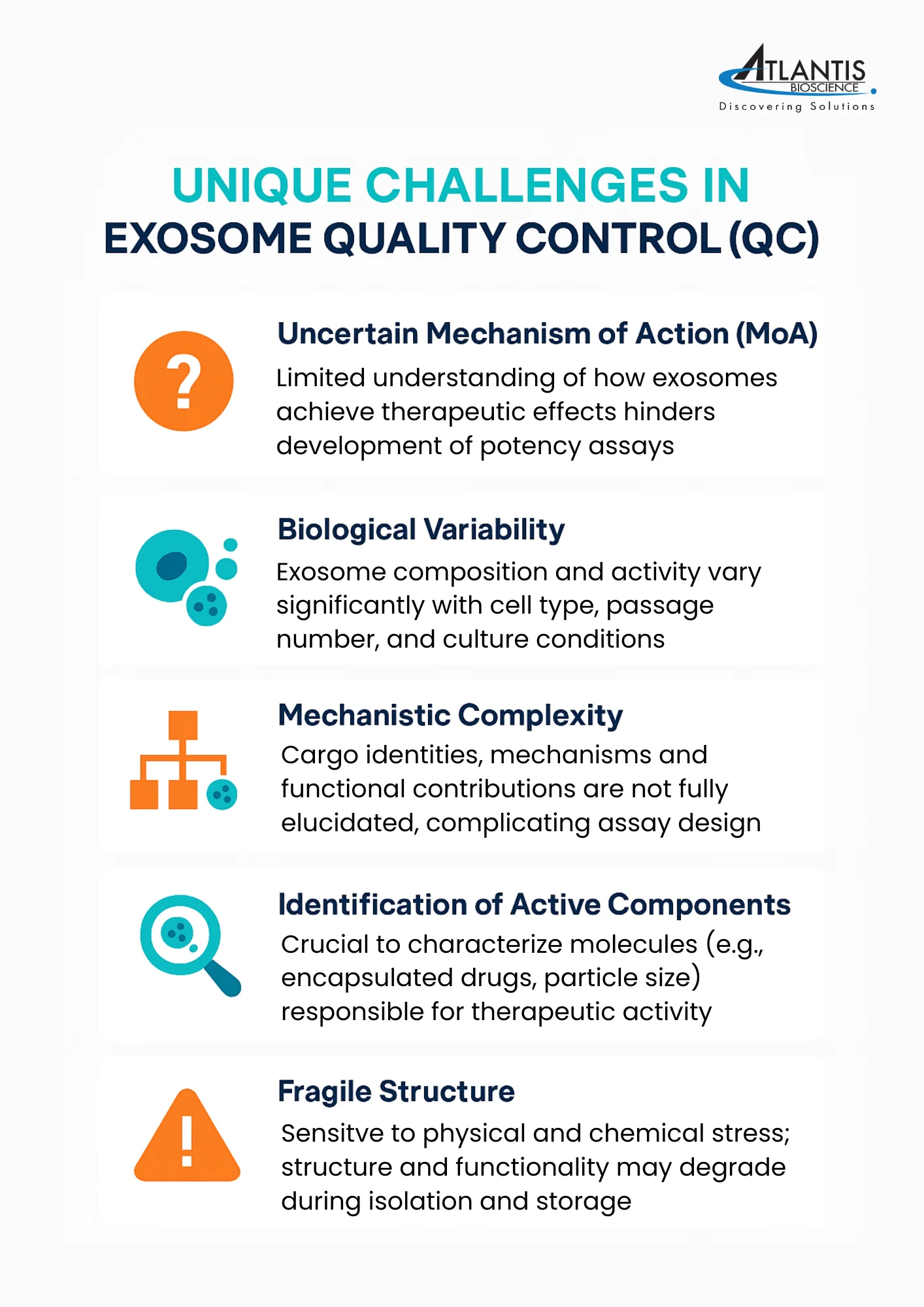
Unique Challenges in Exosome Manufacturing
The vesicular nature of exosomes and their origin from living cells increase the complexity of sterility assurance. Unlike small molecules, EVs are sensitive to standard sterilization procedures (e.g., filtration through 0.22 µm filters may retain or damage EVs), which limits terminal sterilization options. This makes aseptic processing and in-process microbial control even more critical.
Mycoplasma Risk Is Underappreciated
Mycoplasma contamination is common in academic labs and may go unnoticed due to its small size and lack of turbidity in culture.
Routine mycoplasma testing (e.g., PCR-based or culture-based per EP 2.6.7) must be incorporated into the manufacturing and QC process.
For exosomes derived from immortalized or stem cell lines, ongoing mycoplasma surveillance of the cell bank and master working cell banks (MCB/WCB) is mandatory.
Timing of Testing
Sterility and related biosafety testing must be incorporated at both the drug substance (DS) and drug product (DP) stages. Early-phase products may be tested in batch mode (end-product testing), while later stages should implement real-time in-process controls to meet current Good Manufacturing Practice (cGMP) expectations.
Rapid Sterility and Mycoplasma Testing
For clinical trial timelines, rapid microbiological methods (RMMs), such as PCR-based or ATP bioluminescence assays, are gaining interest as acceptable alternatives to traditional 14-day sterility tests. These methods offer shorter turnaround while maintaining sensitivity, though their use must be validated and justified to regulators.
Viral Safety and Raw Materials
Viral safety evaluations should also consider the use of animal- or human-derived raw materials (e.g., serum, enzymes). Sourcing from certified suppliers and incorporating viral inactivation/removal steps (e.g., low pH treatment, nanofiltration) are part of a comprehensive viral clearance strategy.
Batch Release and QC Integration
Sterility results are often a prerequisite for product release. As exosomes are highly sensitive to processing and storage conditions, integrating QC checkpoints at harvest, formulation, and fill-finish steps helps ensure batch consistency and sterility.
Sterility Test Method Validation
USP <71> sterility tests must be validated for each product matrix, including exosome formulation buffers, which may interfere with microbial growth detection. Academic protocols may use culture-based sterility checks informally, but for therapeutic products, a validated sterility test must demonstrate detection of <10 CFU/mL of common contaminants under worst-case conditions.
If the formulation contains preservatives or antimicrobial excipients, their neutralization must be validated as part of the test.
Viral Safety Testing and Source Material Risk
Academic labs often use fetal bovine serum (FBS) or human serum, which are potential sources of adventitious viral contamination. Therapeutic-grade exosome production must use qualified, virus-screened, and traceable raw materials, or shift to serum-free or xeno-free culture systems.
Viral safety testing may involve:
Aseptic Process Design and GMP Compliance
In academia, exosome isolation often occurs in open systems (e.g., ultracentrifugation, manual pipetting), which are unsuitable for GMP production. Researchers should plan early for closed or functionally closed systems (e.g., TFF with sterile connectors) and aseptic processing under Grade A/B cleanroom conditions, as sterility cannot be achieved through terminal sterilization. It is advisable to engage with a GMP-experienced partner or CDMO early to map out a compliant aseptic manufacturing process.
Since aseptic conditions are critical, regular environmental and personnel monitoring during production is required to demonstrate continued control of the cleanroom environment.
Environmental Monitoring and Contamination Control
In non-GMP academic settings, the working environment is rarely monitored for microbial burden.
When scaling toward therapeutic use, environmental monitoring (EM) plans should be implemented—monitoring air, surfaces, and personnel.
Documentation of cleanroom control and microbial recovery logs will be expected in regulatory filings.
In early-stage development of biologic products, a practical approach to quality control is often taken. Standard operating procedures are used to promote consistency across manufacturing runs. Batch-to-batch comparability is typically assessed by comparing newly produced exosomes against reference batches using a combination of biochemical, biophysical, and functional assays.
Transitioning from academic protocols to regulatory expectations often requires:
The FDA requires that sterility and biosafety assessments for biologics follow guidelines such as the United States Pharmacopeia (USP) <71> for sterility testing, <85> for endotoxin testing, and ICH Q5A for viral safety evaluation. These standards are adapted and reinforced for Advanced Therapy Medicinal Products (ATMPs), including exosome therapeutics

For academic innovators leading the development of exosome-based therapeutics, one of the most critical quality control challenges lies in accurately defining what has been isolated.
These nanoscale vesicles are a subtype of EVs and often share overlapping physical and biochemical features with other EV populations. This similarity makes it technically difficult to distinguish exosomes with certainty, yet such precise characterization is essential to ensure reproducibility and enable clinical translation.
Although proteomic analyses have identified a range of proteins frequently detected in exosome preparations, it is increasingly recognized that these markers are not exclusive to exosomes. Instead, they are more accurately described as “exosome-enriched” rather than “exosome-specific,” as various EV subtypes often carry overlapping molecular signatures.
To bring more clarity and standardization to the field, the International Society for Extracellular Vesicles (ISEV) has proposed minimal criteria for exosome identification. These include the detection of two key protein categories:
When isolating exosomes from complex biological fluids such as serum, plasma, or urine, researchers must also evaluate sample purity. This involves checking for the presence of non-vesicular contaminants, such as albumin or apolipoproteins, which can co-purify with EVs and potentially skew downstream analyses or functional readouts.
For academic labs developing early-stage exosome technologies, establishing rigorous characterization protocols not only enhances the scientific robustness of their findings but also builds a foundation for future regulatory compliance and clinical scalability. A clear understanding of the strengths and limitations of available analytical tools—as outlined in the table below—is essential for designing quality control strategies that can withstand scrutiny from both peers and regulators.
| Purpose | Methods | Advantages | Disadvantages |
| Detection of exosomal morphology | Electron microscope | Offers high-resolution imaging of internal structures and particle size distribution. | TEM (transmission electron microscopy) – Complex Sample Preparation – Unsuitable For High-Throughput Analysis. SEM (scanning electron microscopy) – Simpler to operate and better suited for Surface Morphology, but its resolution is Lower Than TEM -Less Effective for small particle analysis. |
| Detecting the size of exosomes | Dynamic light scattering technology | Measures exosome size with a lower detection limit of 10 nm (Ideal for monodisperse samples) | – Unsuitable for heterogeneous exosome populations – Cannot determine concentration – Cannot distinguish protein contaminants. |
| Detecting the size and concentration of exosomes | Nanoparticle Tracking Analysis Technology (NTA) | – Fast, real-time exosome observation – Higher resolution than flow cytometry (detection limit of 30–40 nm) | – Involves complex operation – Cannot clearly distinguish protein contaminants – Sensitive to camera settings and detection thresholds. |
| Detection of biomarkers of exosomes | Flow Cytometry | – Fast high-through put multi-channel analysis with low sample concentration required | – Labor-intensive, – Has a detection limit of 400 nm – Cannot measure exosome size accurately – Optical limitations and low resolution reduce its effectiveness for polydisperse, low-refractive samples. |
| Detection of expression of exosomal marker proteins | Enzyme-linked immunosorbent analysis (ELISA) | – High specificity and rapid – High-throughput analysis of marker proteins – Both qualitative and quantitative | – Time-consuming – Prone to poor repeatability and interference |
| Western Blot | – Well-established method – Enables qualitative and quantitative analysis of exosome marker proteins | – Time-consuming – Less suitable for detecting markers in biological fluids due to variability by cell type. |
Manufacturing exosomes at clinical and commercial scales poses unique challenges:
Understanding the mechanism of action (MoA) is essential for clinical translation. As with any biologic, regulators will require evidence of therapeutic effect, MoA, and batch-to-batch consistency. This includes:
| Attribute | Criteria |
| General properties | SizeMorphologyParticle numberRNA concentrationSurface marker |
| Safety | Mycoplasma Bioburden Adventitious virus)Sterility Endotoxin |
| Identity | Active pharmaceutical ingredient |
| Impurities | Host cell protein/DNA |
| Potency | Based on Mechanism of action (MoA) Assay |

Academic labs are driving innovation in exosome therapeutics—but without early attention to quality control, safety testing, dosing, and regulatory compliance, these innovations may fail to reach patients.
From preclinical studies through IND submission and GMP production, researchers must build clinically viable, scalable platforms. This means implementing robust analytical and safety testing methods, understanding dosing and biodistribution, and developing regulatory-grade data packages that support fast-track opportunities.
The path to clinical adoption is complex, but with the right frameworks, academic innovators can lead the charge in translating EV-based therapeutics into safe, effective, and approvable treatments.

Connect With Our Technical Specialist.

Request For A Quotation.

Discover reliable EV labeling beyond PKH. Explore Biotium’s ExoBrite™ stains for accurate, reproducible extracellular vesicle analysis.
Discover how Exoid TRPS delivers precise EV and exosome characterization through real-world case studies in diagnostics, vaccines, and therapeutics.

Liquid biopsy analysis has emerged as a groundbreaking tool in precision medicine, offering a minimally invasive way to detect and monitor diseases through biomarkers found
Contact our Customer Care, Sales & Scientific Assistance
Consult and asked questions about our products & services
Documentation of Technical & Safety Data Sheet, Guides and more...